by Phillip Kindschi | Oct 10, 2013 | Uncategorized
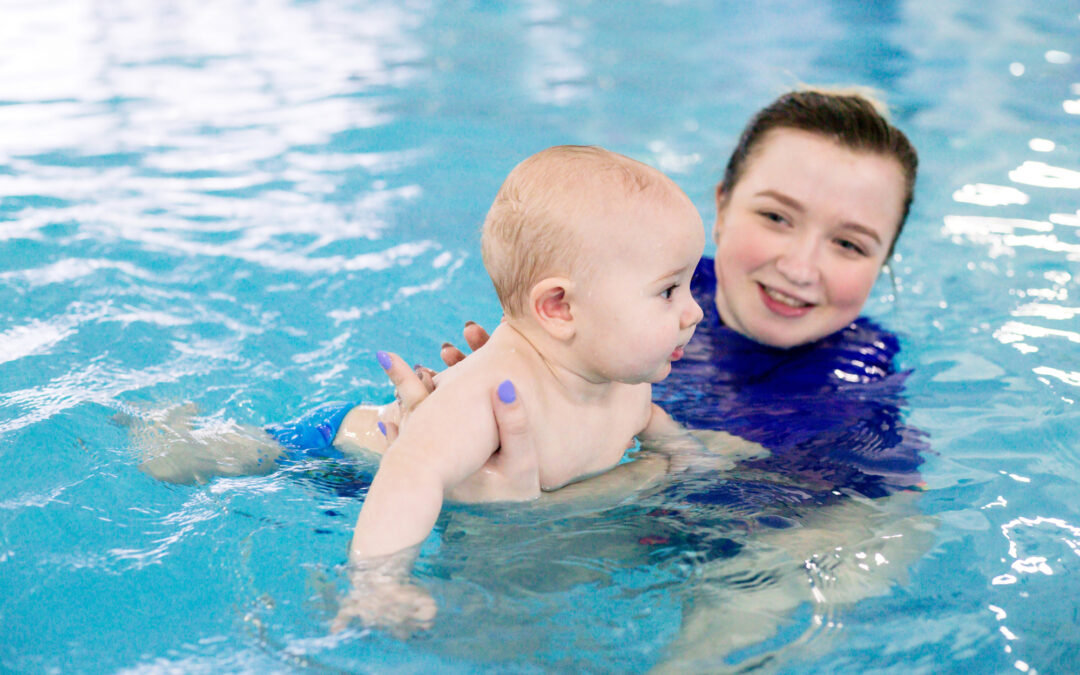
Aquatic therapy is known to be beneficial in physical therapy to address muscle weakness, balance deficits, pain, and decreased flexibility. About a month ago, TherapyWorks started an off campus aquatic therapy program that is allowing some of our patients to enjoy the pool environment. Aquatic therapy sessions are one on one with a therapist, or sometimes even one patient to two therapists if more assistance is required. Each patient has a specialized treatment plan, just like they would in the clinic. We work on similar goals as clinic therapy, just in a different environment.
 Water can make it easier for our patients to move around and they are able to explore different varieties of movement without the limitations of gravity. Those patients who may be in pain due to stress on the joints will find the water especially helpful, with better tolerance for exercising without pain. Aquatic therapy also has secondary benefits of stimulating language and communication, increasing respiratory function, tone reduction, and increased body awareness. For more information on our aquatic therapy program, please speak with your current therapist or call TherapyWorks at (918) 663-0606.
Water can make it easier for our patients to move around and they are able to explore different varieties of movement without the limitations of gravity. Those patients who may be in pain due to stress on the joints will find the water especially helpful, with better tolerance for exercising without pain. Aquatic therapy also has secondary benefits of stimulating language and communication, increasing respiratory function, tone reduction, and increased body awareness. For more information on our aquatic therapy program, please speak with your current therapist or call TherapyWorks at (918) 663-0606.

by Phillip Kindschi | Sep 4, 2013 | Occupational Therapy, Speech Therapy
 Your child’s care and progress is our number one priority at TherapyWorks. We have all heard the phrase “it takes a village”, well it truly does to care for a child with special needs. Do you know who is or should be on your child’s team? For example, did you know that a child with cerebral palsy should be seen by an orthopedic doctor every 6 months to year for hip and spine x-rays because they are at greater risk for dysplasia? Many times families are referred to various specialists without fully understanding what that person’s role is in their child’s care. The following is a list of the most common specialist that may be apart of your child’s team.
Your child’s care and progress is our number one priority at TherapyWorks. We have all heard the phrase “it takes a village”, well it truly does to care for a child with special needs. Do you know who is or should be on your child’s team? For example, did you know that a child with cerebral palsy should be seen by an orthopedic doctor every 6 months to year for hip and spine x-rays because they are at greater risk for dysplasia? Many times families are referred to various specialists without fully understanding what that person’s role is in their child’s care. The following is a list of the most common specialist that may be apart of your child’s team.
Therapist: Occupational Therapist, Physical Therapist, Speech Language Therapist and provide therapeutic services
Orthopedic Physician: Specializes in treating conditions and injuries involving bones and connective tissue, including tendons and ligaments
Neurologist: Specializes in study, diagnosis and treatment of injury and disease of nervous system. These include brain, spinal cord, muscles and nerves throughout body.
Pediatrician: Specializes in the medical care of infants, children, and adolescents The age limit usually ranges from birth up to 18 years.
Developmental Pediatrician: Developmental pediatricians focus on developmental, behavioral and learning
issues from infancy through young adulthood
Geneticist: Evaluate, diagnose and manage patients with heredity conditions or congenital malformations
Vision Therapist: Also known as vision training. This treatment is used to improve vision skills such as eye movement
control, eye coordination and teamwork. This is performed under supervision of optometrist, or orthoptist
ENT: An ear, nose and throat doctor specializes in diagnosis and treatment of disorders of the ear, nose, sinuses, throat, face and neck.
Psychologist: This specialist evaluates, diagnoses, treats, and studies behavior and mental processes. Clinical psychologists and school psychologists work with patients in a variety of therapeutic contexts
Psychiatrist: Psychiatrists are medical doctors who must evaluate patients to determine whether or not their symptoms are the result of a medical illness, a combination of medical and mental, or a strictly mental one
If you are unsure if your child should be seeing one of these specialist please consult with your therapist and pediatrician for a recommendation. It is very important that if your child is seeing one of these specialists that you please inform your therapist so that they can collaborate and be informed of and changes in plan of care.

by Phillip Kindschi | Jul 2, 2013 | Uncategorized
Summertime Fun with PT
It’s summertime and one of the best times for kids to go outside and do some activities to build important gross motor skills, strengthen muscles, increase balance and coordination, motor planning and endurance. There are all kinds of things they can do outside like the regular activities of riding a bike, running, jumping rope, skipping, galloping, jumping on the trampoline, playing on the swing set and going to the park.
Summer is a great time, but if it gets too hot outside, just jump in the pool and cool off with a swim. Running through the sprinkler and tossing water balloons are other fun activities to stay cooled off. Swimming is a great way to strengthen those muscles and make them work without the kids even knowing it.
Here are some more great activities that your child (and you) can do to help increase strength, balance, coordination, motor planning, endurance and overall gross motor skills:
- Younger kids love bubbles! Blow some bubble and have them stomp the bubbles, making sure that they use both the left and the right foot to stomp. Then blow some bubbles high and have them reach for them where they are standing on their tip toes. Chasing bubbles is also a great activity.
- Make hopscotch out of sidewalk chalk. Make sure when your child is hopping on one foot they alternate, one time with the left foot and then one time with the right foot.
- Walking on the curb with one foot in front of the other or draw a straight line with sidewalk chalk and walk the line with one foot in front of the other.
- Scavenger hunts are good for all ages. You can put the clues:
-
- Down low so the child has to squat and then stand back up
- Up high so the child has to reach on their tip toes
- Where they have an obstacle that they have to step over or climb over
- Where they have to climb up and down a couple steps
- Where they have to walk on uneven ground such as grass, gravel, sand, etc.
- Obstacle courses – make them fun with simple things you have around the house. Here are couple of ideas:
- Fill plastic bottles with water and put them in a zig zag pattern to run or hop through
- Jump over soft pool noodles or a garden hose
- Use a board or garden hose as a tightrope
- Crawl through boxes or army crawl across a blanket or sheet
- Toss balls or beanbags into a basket or bucket
- Kick a ball at a target (alternating feet when kicking)
- Set hula hoops down and jump from hula hoop to hula hoop
- Run, skip, gallop, run backwards, crab crawl, bear crawl
- Use Frisbees, horse shoes, bouncy balls, etc.
- Put a broomstick across a couple chairs to go under or do the limbo
There is so much to do outside, just make it fun and enjoy! Check out some summertime sensory ideas
here!

by Phillip Kindschi | Jun 10, 2013 | Uncategorized
Commonly referred to as being “pigeon toed,” in-toeing is when a child walks with his or her feet turned inward. In-toeing can cause a child to seem more clumsy, demonstrate poor balance, and to trip and fall more frequently than peers. The cause of in-toeing can be the result of a few different factors.
- In-toeing can be due to the ankles and/or feet themselves being curved inward
- In-toeing can be the result of tibial torsion where the bones in the calves twist inward causing the feet to appear to turn inward when walking.
- In-toeing can be the result of femoral torsion where the long bones of the thigh twist inward causing the knees and feet to point inward.
- In-toeing can also be the result of shortened muscles in the ankles or hips.
As mentioned in last month’s blog on W-sitting, when children sit in a W this can result in shortened muscles in the hips which can lead to in-toeing. Children who chronically sit in a W create excessive range of motion in their hips in one direction, while also creating a decreased range of motion in their hips in the opposite direction. This imbalance in the muscles surrounding the hips can make them very tight and can cause the entire leg to turn inward.
A physical therapist can help by assessing a child to determine which of these problems are causing the in-toeing. Depending on the cause of the problem a physical therapist will recommend the proper course of action, which may include:
 Orthotics for proper positioning of the feet and ankles.
Orthotics for proper positioning of the feet and ankles.- Stretching for tight muscles.
- Strengthening for weak muscles.
- De-rotation bands, which are elastic bands that help reposition in the legs in proper alignment.
- Eliminating W sitting in favor of sitting in criss-cross.
by Phillip Kindschi | Feb 21, 2013 | Occupational Therapy, Physical Therapy, Physical Therapy, Physical Therapy, Physical Therapy, Physical Therapy, Physical Therapy, Speech Therapy
It’s often said it takes a village to raise children. With children with special needs, that village sometimes includes a number of
therapists and specialists.

When children are brought into our clinic for their first assessment, the therapist may request additional assessments from other health care professionals. This allows therapists and parents to get a clearer picture of the child’s strengths and weaknesses and gives valuable information about how to best address the child’s individual needs.
Parents may feel overwhelmed or confused about these many specialists and may ask, “What does that person really do? Why is my child meeting with them?” Below is a basic review of some of the specialists your child may see and their unique role in your child’s treatment team.
At TherapyWorks, your child’s therapy team may include:
Speech-language pathologists give children the skills necessary for successful communication and meaningful interactions with others. Additionally, speech therapists assist children with feeding difficulties to eat and swallow safely.
Physical therapists work to improve muscle strength, range of motion, reflexes and coordination. Our physical
therapists are also trained to fit and cast custom foot orthotic devices. Orthotic supports align the foot or lower leg and improve posture, sitting, standing, walking and running.
Occupational therapists help children develop or regain skills necessary for play and work, and self and home care. Children may also need occupational therapy to help them with school and social skills. Play is important for a child’s mental, physical and emotional development. Occupational therapists also address sensory processing and integration problems which have a tremendous impact on motor skills, behavior, learning and a child’s ability to process information and respond to the demands and changes of daily living.
We also work with the following outside professionals to create a total treatment plan for your child:
Physicians emphasize the physical health of the child including height, weight gain, and absence of disease. Doctors also work closely with dieticians or nutritionists to ensure your child’s nutritional needs are being met for optimal growth and
development.
Psychologists and mental health professionals help people learn to cope with the daily stresses of life. For many of our families, psychologists provide strategies to help manage behavior issues to make children more successful at home and school. They also perform standardized assessment of developmental milestones.
Teachers and administrators address the educational/academic needs of children and work to meet educational mandates as required by state and federal laws.
Communication Intervention Birth to Three- 2nd Edition by Louis M Rossetti.
Delmar Publishing 2001 was referenced.
by Phillip Kindschi | Feb 12, 2013 | Uncategorized
We’ve all seen it. Kids sitting on the floor with their knees bent, feet and toes pointed and legs out to each side, in a “W” position.
WHY do some children sit in this position?
Kids like to sit in a W because it’s easier. W-sitting creates a wide base of support, the child uses fewer muscles and it’s almost impossible to fall over when sitting in a W-position. Once a child learns to sit in a W-sitting position, it becomes a habit very quickly.
WHEN does W-sitting become a problem?
Consistent W-sitting can lead to orthopedic problems as your child gets older. Hip dislocation, twisting of the bones and shortened muscles in the hips and feet are some of the complications caused by W-sitting. In W-sitting, the child is unable to properly rotate his trunk which can cause delays in skills, such as crossing midline and transitioning from sitting to crawling to standing.
In addition, persistent W-sitters can become pigeon-toed because of the stress on the joints and shortened muscles that develop. (Look for more information on pigeon-toes in next month’s PT blog!). In worst case scenarios, surgery is required to fix the joints or to lengthen shortened muscles. It is easier to never let your child start W-sitting.
WHAT should I do if my child already is a W-sitter?
Try to work on other sitting positions such as criss-cross, longsitting (legs in front), and side sitting. You may have to remind him to move his legs to a different position. It will take a lot of repetition to correct the sitting position, but it will decrease the chances of complications in the future.
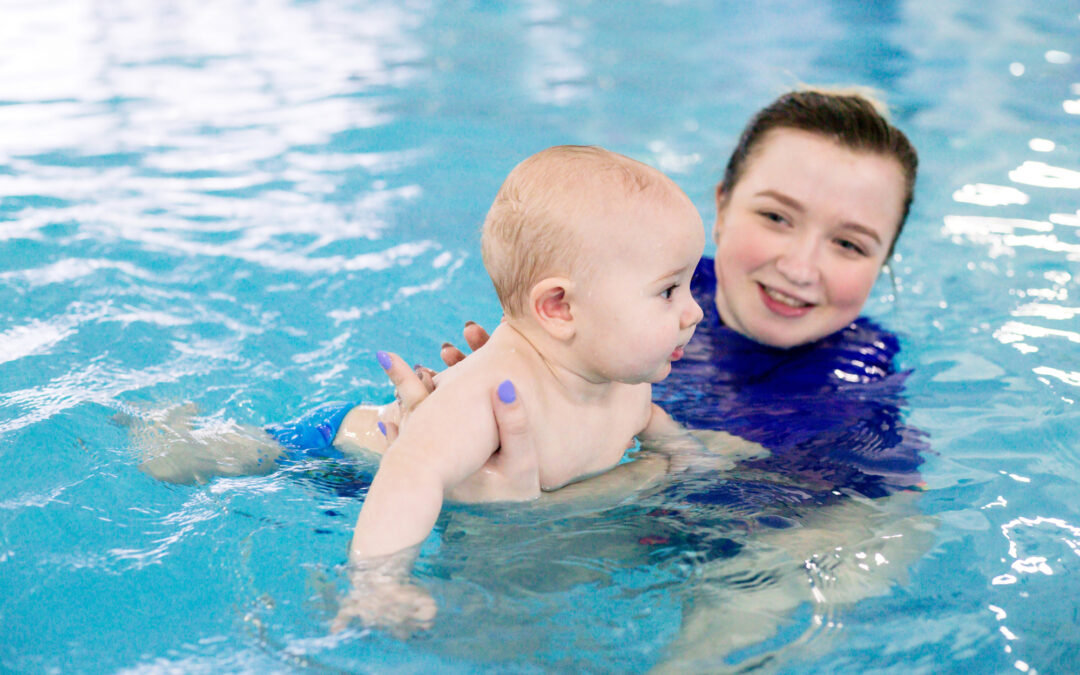
 Water can make it easier for our patients to move around and they are able to explore different varieties of movement without the limitations of gravity. Those patients who may be in pain due to stress on the joints will find the water especially helpful, with better tolerance for exercising without pain. Aquatic therapy also has secondary benefits of stimulating language and communication, increasing respiratory function, tone reduction, and increased body awareness. For more information on our aquatic therapy program, please speak with your current therapist or call TherapyWorks at (918) 663-0606.
Water can make it easier for our patients to move around and they are able to explore different varieties of movement without the limitations of gravity. Those patients who may be in pain due to stress on the joints will find the water especially helpful, with better tolerance for exercising without pain. Aquatic therapy also has secondary benefits of stimulating language and communication, increasing respiratory function, tone reduction, and increased body awareness. For more information on our aquatic therapy program, please speak with your current therapist or call TherapyWorks at (918) 663-0606.

 Your child’s care and progress is our number one priority at
Your child’s care and progress is our number one priority at 








